Malaria Control

At Health Access Sumbawa (HAS), we’ve been tackling the persistent challenge of malaria since 2015. Despite significant global efforts to combat this disease, it continues to be a serious issue, especially in remote communities. In regions like Sumbawa, essential anti-malarial drugs, though available, often remain unused in regional hospitals, while nearby communities, particularly pregnant women and children, suffer from malaria during the rainy season. Tragically, in such areas, up to 20% of children are either lost to malaria or endure lifelong disabilities from it before their tenth birthday. This reality hinders not only individual health but also the broader economic and social development of these communities.
Malaria, caused by Plasmodium parasites and transmitted through the bite of infected female Anopheles mosquitoes, is particularly prevalent in Eastern Indonesia, including the P. vivax and P. falciparum species. The latter, responsible for severe, life-threatening malaria, poses a significant health risk.
Currently, there’s no vaccine for malaria, but successful elimination in many developed and increasingly in developing countries has been achieved through prevention strategies, rigorous infection monitoring, and universal access to diagnosis and treatment. With 70% of Indonesians living in areas with low infection rates, primarily on densely populated islands like Java and Bali, Indonesia aims to be malaria-free by 2030. However, reaching this goal requires intensified efforts to serve remote, under-served communities, particularly in eastern Indonesia.
Diagnosing malaria typically involves blood smear slides examined under a microscope. While rapid diagnostic tests (RDT) offer quicker results with less training, they are more costly and less reliable than microscopy, making them unsuitable for mass screening.
When HAS began its initiative in the north coast of Cempi Bay, there was no malaria control program in place. Our initial steps involved engaging with community leaders, organizing volunteers, and conducting a complete village census, including numbering each home for efficient patient tracking. Our team of community volunteers distributes and installs treated bednets, ensuring every individual has protection while sleeping. All our programs, including the bednets, are provided at no cost to the public.
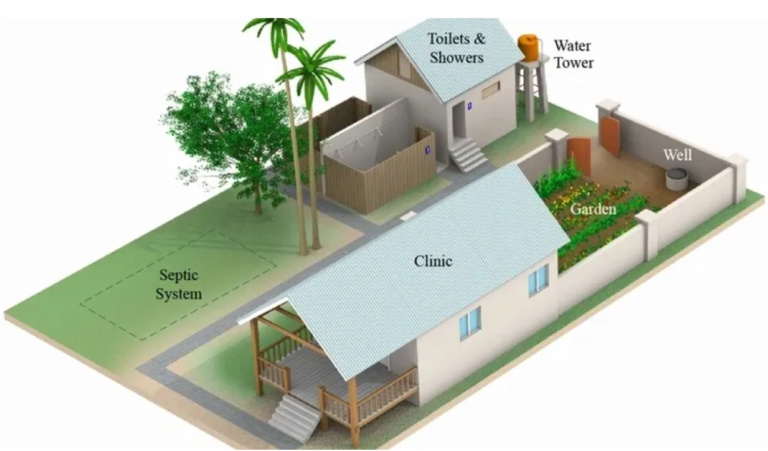
In 2016, we established a laboratory and health clinic in Sili village, enabling competent malaria diagnosis and treatment. Two health department staff members were trained at The Sumba Foundation Malaria School, becoming Sumbawa’s first-ever WHO-certified malaria microscopists.
HAS’s approach to malaria control focuses on eliminating the parasite in humans through universal screening and effective treatment, thereby neutralizing the mosquito vector. This strategy avoids the need for insecticide spraying, yielding environmental, health, and cost benefits.
Our clinic, staffed by three part-time nurses and an administrator, has successfully controlled malaria in three remote hamlets, protecting around 1,000 people as of November 2017. This accomplishment is a testament to our commitment to making a tangible difference in the lives of those in hard-to-reach communities.
Scaling Up Our Malaria Control Program
HAS Triples its Bed Net Program +/- $16,500
In 2019-2020 we took a major step toward eliminating malaria in 3 towns called Mata, Panco & Tolo’oi. These communities are adjacent to the area we have been serving since 2015. Mata is the largest village. 1,500 people / 350 homes. In November 2019 we completed the census, numbered every home, and covered every bed in Mata with long lasting treated bed nets.
In December the HAS Team hung nets in Panco, a small roadless hamlet one hour boat ride from our clinic. Tolo’oi received nets and house number plates in February 2020. Tolo’oi has 852 residents / 292 homes.
Without a vaccine, malaria control is a battle that never The original 600 bednets we placed 5 years ago are in tatters today. These will have to be replaced in November 2021, before the start of the next rainy season, at a cost of about $6,000 for the materials alone. We have won the battle against malaria, but the war goes on.
Malaria Control Photos
Lots More To Do
Expanding Our Service Area
We run our own programs in our primary service area, the dark blue area on the map below. This covers an area within 1 hour from our clinic. We provide consulting and make grants to change-makers in a much larger area, primarily within the bright green area on the map. However, our influence is not limited to Sumbawa. We have sponsored worthy public health, nutrition, and education initiatives as far away as the island of Bali, a one-hour flight to the west.


